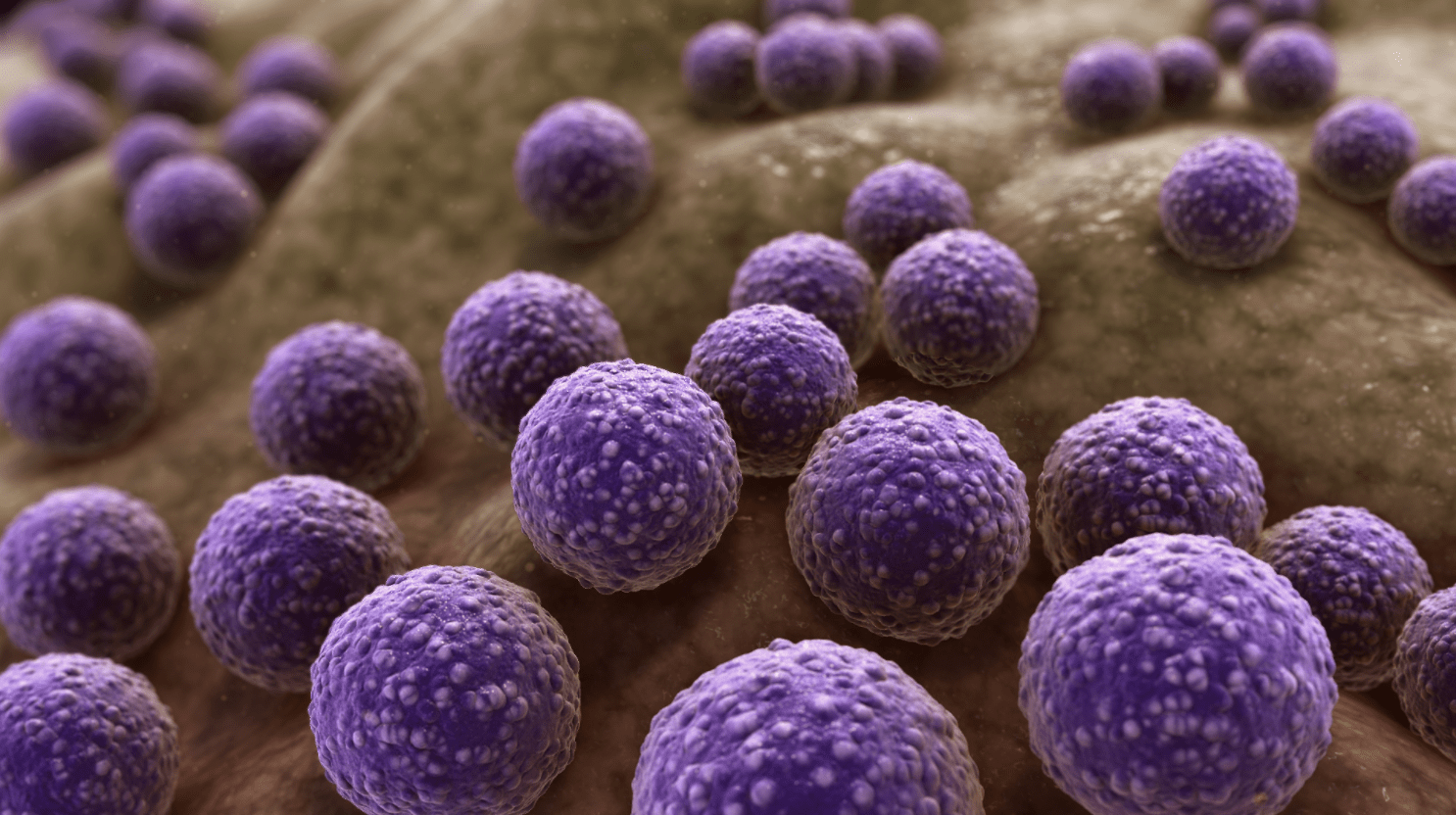
One of the first things I learnt in pharmacy school, particularly in Pharmaceutical Microbiology, was that “microorganisms are ubiquitous.” I learnt this under the topic, The Ubiquity of Microorganisms. It was also the first time I ever heard the word “ubiquitous”. That microorganisms are ubiquitous simply means that microorganisms are everywhere.
Why such a big word for a simple definition, I thought. The definition may be simple, but the issue of antibiotic resistance is not. Antimicrobial resistance is rising dangerously, globally. This may not be unconnected to the fact that microorganisms are ubiquitous and can adapt to or survive the harshest conditions.
Antibiotic Resistance and Antimicrobial Stewardship
Before the discovery of antibiotics, infectious diseases were responsible for high morbidity and mortality rates globally; the average life expectancy was 47 years. However, there came Alexander Fleming, who thankfully saved the day with his Penicillin discovery.
Now, decades after the first clinical use of antibiotics, we seem to be going back in time; infections have once more become a threat, no thanks to the rise of resistant bacteria. So terrible are the consequences of resistant bacteria that health experts report that we are heading for a post-antibiotics era, where infections will be harder to treat. Worse is the decline in the rate of developing and approving novel antibiotics.
These devastating trends contribute to the World Health Organisation declaring antimicrobial resistance as one of the top 10 global public health threats humans face. It is also why it became crucial to have people responsible for conserving antibiotics and upholding their judicious use. Thus, the concept of antimicrobial stewardship started.
Antimicrobial stewardship is a set of coordinated activities designed to guarantee the optimal choice of therapy for patients that achieves the best clinical outcome, while reducing toxicity. It aims to prevent the overuse, abuse and inappropriate use of antibiotics and to reduce the development of resistance at patient and community levels.
It is tempting to associate antibiotic resistance with the proverbial hungry goat owned by an entire village which starves to death because it has no specified owner. However, unlike the goat, the issue of antibiotic resistance has a designated steward.
A steward looks after something entrusted in his care with a responsibility to manage it. By default, all healthcare professionals are antimicrobial stewards. However, pharmacists are responsible for setting up antimicrobial stewardship programmes in their respective healthcare facilities and ensuring the success of such.
Specific Roles of Pharmacists
Antimicrobial stewardship (AMS) optimises antibiotic use across every healthcare setting. As pharmacists, we are core AMS team members and play a vital role in achieving AMS goals throughout the continuum of care, whether in-patient, out-patient or long-term care sectors. We are drug custodians, who are well-placed to lead campaigns and ensure that health facilities meet regulatory requirements that facilitate antimicrobial stewardship.
Pharmacists are in a great position to initiate a structured antimicrobial stewardship programme in healthcare facilities (where there is none). All AMS programmes involve a multidisciplinary team of pharmacists, doctors, nurses, infectious disease specialists, etc., and a concrete programme. Pharmacists can spearhead this initiative.
Pharmacists are advocates and influencers who improve public knowledge and attitude towards antibiotics. For example, community pharmacists are the first point of contact for the healthcare-seeking community because of the ease of accessibility. So, they are in a great place to alter public perception about antibiotic use.
Pharmacists are intervention experts who optimise prescriptions wherever they are. Whether in the hospital or community, pharmacists review prescriptions and intervene where necessary.
In hospitals, it is a good idea to combine restrictive interventions (interventions that set a limit on prescribing antibiotics) with persuasive interventions (interventions that advise physicians on prescribing or give feedback about a prescription based on the restrictive limits set).
In healthcare facilities, pharmacists promote strict adherence to medication guidelines (an example is the provision of guidelines on antibiotic dosing regimens). They monitor antibiotic use (dosage adjustment in a case of organ dysfunction or in cases of super drug resistance, where higher doses of antibiotics may be required). Pharmacists should also spearhead an annual or quarterly antibiotics review in health facilities.
Pharmacists are teachers and educators who provide education and information to other healthcare professionals. They put together clinical conferences and training, newsletters and articles. Topics range from antimicrobial stewardship to antimicrobial use and resistance.
They also educate patients, caregivers and members of the public who come in contact with the healthcare system.
The role of pharmacists as antimicrobial stewards is as ubiquitous as the microorganisms we try to control. Everywhere a pharmacist is, there is a role to play in pushing back against these resistant microorganisms that threaten the efficacy of antimicrobials.
Special Note: Christmas and Antibiotic Use
It has been observed by yours truly that there is a positive association between festive seasons and increased consumption of antibiotics. There are more clients or patients who want one antibiotic or the other to flush their system or stop their stooling. So, be on your guard and have the right response when they come knocking.










