Worried by the surge in prevalence of cervical cancer in the country, with over 36 million Nigerian women above age 15 at risk of coming down with the condition and 22 deaths recorded daily from the disease, medical experts have called for increase in vaccination of young girls, screening and awareness creation about the disease.
They identified cervical cancer as the second most common cancer and second to breast cancer among Nigeria’s female population, with 12,000 cases diagnosed annually and 8000 annual deaths, which can also be translated as 33 new cases and 22 deaths from the disease daily.
Causes of cervical cancer
Cervical cancer is caused by the Human Papillomavirus (HPV) infections more often than none. HPV, the scientists said, is the most common sexually acquired infection and often impacts young adults who become sexually active early in their lives. While there are high-risk HPV and those with low risk, there is also evidence linking HPV with cancers of the anus, vulva, vagina, penis and oropharynx, they stated.
This explains why the World Health Organisation (WHO) has named January as Cervical Cancer Awareness Month, to raise awareness about cervical cancer and HPV vaccination. This year, the theme of the campaign is “Ending cervical cancer within a few generations”To end the scourge of the disease, the apex health agency saddles women with three tasks of getting informed, getting screened and getting vaccinated. It urges women and girls to get informed by finding out facts about cervical cancer and the HPV that causes it.
Prevention of cervical cancer
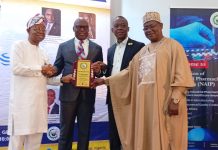
In stemming morbidity and mortality from the deadly condition, the experts including Professor Oliver C. Ezechi, director of research and consultant obstetrician and gynaecologist, Nigeria Institute of Medical Research (NIMR); Professor Juliet Iwelunmor, College for Public Health and Social Justice, Saint Louis University Missouri USA; Professor Joseph D. Tucker, University of North Carolina Chapel Hill, USA and Dr Ucheoma Nwaozuru, Wake Forest University School Medicine, flagged-off a cervical cancer prevention project in Nigeria, tagged ACCESS –HPV.
Fielding questions from journalists at the official commissioning of the project, held in NIMR on Wednesday, Prof. Ezechi, noted that cervical cancer is one of the most preventable and successfully treatable forms of cancer if detected early and managed effectively.
“ Like many cancers, the earlier cervical cancer is detected, the higher the chances of survival” he said.
Inequitable access to HPV vaccination
He however attributed high prevalence of the disease in Nigeria and the resultant number of deaths occurring in women to poor access to effective and inadequate treatment and services. “The inequity in access to service has been attributed to compering healthcare priorities, insufficient financial resources, weak health systems, and limited numbers of trained service providers”, he observed.
To bridge the gap in vaccination for HPV, which is hitherto only available in private facilities, he said their research project- Actions for Collaborative Community Engaged Strategies for HPV (ACCESS-HPV), aims at supporting the Nigerian national cancer prevention and control programme, towards achieving its drive to join other nations of the world to eliminate cervical cancer by 2030.
Prof. Iwelunmor, explained the research methodology, saying they are going to explore the bond between mothers and daughters to drive home the message of the importance of HPV vaccination, to improve the uptake of the vaccine.
Iwelunmor, who was represented at the briefing by Chisom Obiezu-Umeh, PhD candidate at SLU College for Public Health and Social Justice, said “In this project, our team will utilise the special bond between mothers and their daughters to improve HPV vaccination of young girls and HPV screening for mothers”.
She further revealed other research procedures to actualise their goals, stating that “they will develop new vaccination campaigns for young girls and HPV self-collection campaigns for mothers, using crowdsourcing open calls and participatory learning communities.
“We will also determine the effectiveness of a final campaign on the uptake of HPV vaccination among girls (ages 9 to 14) and HPV self- collection among mothers (ages 30 to 49) using a stepped wedge randomised control trials”.
.