A recent study by the Swiss Tropical and Public Health Institute (Swiss TPH) has revealed that resistance to the World Health Organisation’s (WHO) newly endorsed multidrug-resistant tuberculosis (MDR-TB) treatment regimen is already being transmitted directly between patients.
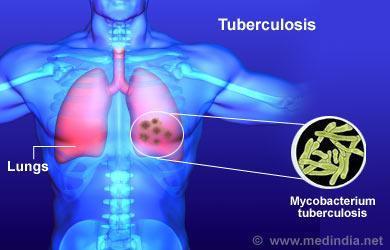
The research, published in the New England Journal of Medicine, analysed nearly 90,000 Mycobacterium tuberculosis genomes from various countries. Among the 514 highly drug-resistant strains identified, 28 percent were found to be transmitted directly between individuals. These strains exhibited resistance to both older and newer treatment regimens and were present across 27 countries.
In 2022, WHO endorsed the BPaLM regimen, a six-month oral treatment combining bedaquiline, pretomanid, linezolid, and moxifloxacin— based on clinical trials, it reported an 89 percent success rate, significantly higher than the 52 percent success rate of older regimens.
Recommended by WHO, the BPaLM regimen aimed to reduce treatment duration, improve efficacy, and lower costs compared to the older, longer treatment regimens.
However, the emergence and transmission of resistant strains pose a substantial challenge to this advancement.
Sébastien Gagneux, head of the department of Medical Parasitology and Infection Biology at Swiss Public Health institute, emphasised the need for increased vigilance staing, “It was crucial to study how Mycobacterium tuberculosis would react to its global roll-out, and now we know that resistance is emerging and being transmitted, which is worrying.”
Gagneux stressed that to avoid a post-antibiotic era; the world must stay ahead in the constant race between drug development and bacterial resistance to prevent a ‘post-antibiotic era. “The rise of highly resistant TB strains is a stark reminder of this challenge,” he added.
Chloé Loiseau, a postdoctoral collaborator at the Swiss Health institute and co-author of the paper, stated, “These new drugs have taken many years to develop, and to prevent drug resistance from emerging, however, it is essential to combine the deployment of these new regimens with robust diagnostics and surveillance systems.”
According to health reports, tuberculosis still remains a global health burden, with approximately 1.3 million deaths in 2022. Nigeria, in particular, has the highest number of TB cases in Africa, with over 350,000 notified cases in 2023 and a rise in drug-resistant TB cases from 2,897 in 2021 to 3,932 in 2022.
The findings of this study highlight the critical need for new treatment regimens with effective diagnostic and surveillance mechanisms to combat the evolving threat of drug-resistant tuberculosis.











