During my time in community pharmacy practice, I collaborated with a TB support organisation that had partnered with medical laboratories to offer free TB testing. Their request was simple: could we direct patients with a persistent cough lasting over two months to these labs for screening?
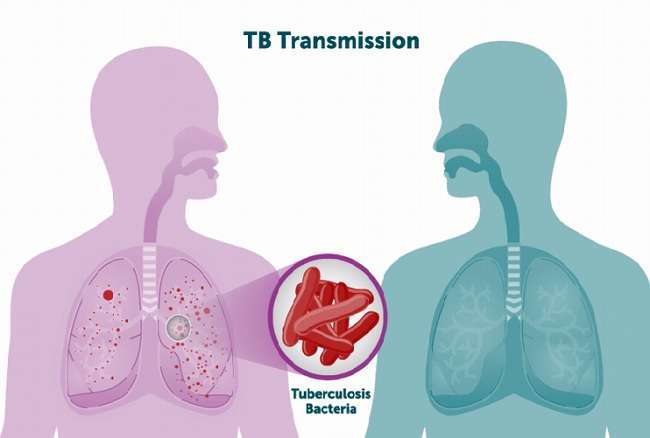
It seemed like a reasonable arrangement. However, we quickly discovered that no one wanted to undergo a TB test. Patients would either never return or insist, after a while, that their cough had disappeared. They feared the stigma associated with a TB diagnosis. This reluctance not only delays diagnosis but also perpetuates the spread of the disease.
- Treatment adherence
TB treatment is notoriously lengthy, often lasting over six months. This prolonged regimen presents significant challenges for patients, leading to poor adherence. Incomplete treatment can result in treatment failure and the emergence of drug-resistant TB strains.
- Drug resistance
Multidrug-resistant TB (MDR-TB) is a growing public health crisis. Resistance to first-line anti-TB drugs complicates treatment, requiring longer, more expensive, and more toxic regimens. In 2022, an estimated 450,000 people developed MDR-TB, highlighting the urgent need to address this issue.
-

Pharm. (Dr) Oyinye Chiekwe Socioeconomic factors
TB disproportionately affects low- and middle-income countries, where overcrowding, malnutrition, and limited access to healthcare accelerate its spread. These socioeconomic conditions create environments where TB thrives, making eradication efforts more difficult.
- Coexisting health conditions
Individuals with compromised immune systems, such as those living with HIV, malnutrition, or diabetes, face a higher risk of developing active TB. These comorbidities complicate treatment and increase mortality rates.
Strategies to mitigate the TB menace
- Enhanced screening and early detection
Mass screening programmes can lead to early detection and treatment, reducing transmission rates. For instance, during my first year at the University of Benin, all new students underwent mandatory medical examinations, including the Mantoux test for TB. Such proactive measures help identify latent TB infections before they become active.
- Shorter treatment regimens
Investing in research to develop shorter, more effective treatment regimens could improve patient adherence and reduce the emergence of drug-resistant strains. Recent advancements have shown promise in this area, but continued support and funding are crucial.
- Addressing social determinants
Improving living conditions, nutrition, and access to healthcare can significantly reduce TB incidence. A multisectoral approach that tackles these social determinants is essential for sustainable TB control.
- Combating stigma
Educational campaigns aimed at reducing the stigma associated with TB can encourage individuals to seek diagnosis and adhere to treatment. Community engagement and support systems play vital roles in this effort.
- Strengthening healthcare infrastructure
Investing in healthcare infrastructure, particularly in high-burden countries, ensures timely diagnosis and treatment. Training healthcare workers and providing essential resources are pivotal steps towards TB elimination.
Conclusion
Tuberculosis remains a formidable global health challenge due to a complex interplay of medical, social, and economic factors. By addressing stigma, treatment adherence, drug resistance, and social determinants of health, we can make significant progress in reducing the burden of TB. Collaborative efforts from healthcare providers, policymakers, and communities are essential to achieving the goal of ending TB once and for all.
By Pharm. (Dr) Onyinye Bridget Chiekwe, PharmD, MScPH, ABMP
pharmbree25@gmail.com











